My name is Dr Cheney Drew, and I am a Research Fellow and Senior Clinical Trials Manager based in Centre for Trials Research in Cardiff University.
About me
Outside of my work at Cardiff University, I have many passions, from ultra-marathon running to arts and crafts, as well as baking cakes. On one occasion, I baked a brain cake for Halloween and was reliably informed by neurosurgical colleagues that this was a faithful, and perhaps disturbing representation of the real thing!
My research
I am involved in the design and delivery of high-quality clinical trials, focusing on neurodegenerative and other neurological disorders. This can involves introducing new medicines, or different ways of using existing medicines to non-medicine based ‘interventions’ such as exercise to try and combat disease.
I am also facilitating BRAIN involve, the public and patient involvement group that helps to inform our research activities.
This year, I worked with Dr Emma Lane to understand the experiences of those who take part in complicated clinical trials for degenerative brain conditions, with a focus on Parkinson’s disease.

Why I’m interested in this area of research
There are two big problems we encounter when running a clinical trial: persuading people to take part (recruitment) and making sure that people continue to participate until the end (retention).
These issues make it more difficult to make firm conclusions about the medicine or treatment being tested because there is not enough data to show that the changes to people taking part are because of the treatment and not due to chance.
We hope that by better understanding the participant experience, we can design clinical trials that make it easier and more acceptable for people to take part in and remain, maximising both recruitment and retention and making sure that the clinical trial has the best chance of providing a definite answer about the treatment being studied.
Our findings
We found that taking part in a clinical trial is a big undertaking for the participant, their partners and close family members, though rewarding on the whole.
Participants said that ongoing communication between them and the research team was extremely important, particularly when the trial finished for them but the results are not available for some time.
Also, the transition from being a participant back to a patient can be really difficult for the participant and that needs to be carefully managed, as well as providing participants with payment for travel and accommodation upfront so they are not left out of pocket.
You may think that some of these considerations are not particularly surprising and are often already factored into clinical trial designs. However, our data has demonstrated that small changes in the way this is managed (i.e. paying for those costs upfront and not requiring the participant to apply for reimbursement) would make the experience much better for participants.
Learn more about the LEARN study
We created some short information videos and accompanying documentation that can be used to support people with Parkinson’s disease in taking part in clinical trials, using the data from our study.
As we move away from the challenges of COVID we have been able to harness the benefits of online tools and reimagine our involvement and engagement delivery. In this article, we shine a light on some of the PPI activities from 2022 – 23.
Our Brain Involve group continues to meet online and this has enabled geographical spread across Wales and plans are ongoing for face-to-face activities in the coming year. Our Brain Involve team have informed and supported grant and fellowship applications for senior scientists and early career researchers.
From Brownies and Cubs, to people living with neurodegenerative diseases in the UK and abroad, our face-to-face engagement programme has made a welcome return. One of our biggest events was a full day of activities delivered to over 300 pupils at two local primary schools.
This formed part of the Radyr and Morganstown Festival and had huge support from Headway Cardiff, a brain injury charity. Everyone got involved in learning about the brain, testing their own brains, brain surgery assemblies and having a bounce on the inflatable brain! Year 6 pupils also produced some beautifully creative pictures and poems inspired by our day and the resources created have now been used in other primary schools.
We have also engaged heavily with the patient community. We have become a driving force, ensuring that patient voices are regularly heard at the Network for European CNS Transplantation and Restoration (NECTAR) conference held this year in Athens in 2022, organising sessions that allow patients to share their voice directly with scientists.
Last November, we held a Huntington’s disease patient and family day, bringing the patient, clinical and scientific communities together to share the research that is going on. Our engagement enables us to build trust with our local communities to then create positive involvement, working with people living with neurodegenerative diseases to shape and inform our science.
One example of our involvement activities this year has been focus groups conducted with people living with multiple sclerosis, discussing their thoughts on genetic testing and their prognosis. We have also worked closely with people with Parkinson’s to create resources to support their participation in clinical trials.
We are delighted to have successfully delivered the UniQure Phase I/II gene therapy trial focussing on knocking down Huntington protein production within neurons in Huntington’s Disease, to three patients in Cardiff. This gene therapy is potentially curative or significantly slowing disease progression in this fatal neurodegenerative disease.
Early results are encouraging and if replicated in the ongoing study will represent a major advance in the treatment of this devastating neurological disease.
As well as being a cutting-edge Gene Therapy, its delivery is minimally invasive, with the complete operative procedure taking place within an MRI scanner so that the delivery targeting can be monitored and performed safely in real-time.
This trial will allow people in Wales access to access innovative Advanced Medicinal Therapeutic Medicinal Products (ATMPs), a core objective of Health & Care Research Wales and of our BRAIN Unit. Given the advanced nature of the neurosurgical techniques involved, this trial will be delivered via our Neurosciences Research Unit (NRU) at University Hospital Wales but will be open to participants across Wales and the UK.
We are currently screening an additional three people to continue the trial. Participants in the UK cohort are also referred from University College London (UCL) as we are the only surgical site in the UK with the MRI stereotaxis delivery system.
The images taken during the UniQure trial have allowed us to 3D model the infusion delivery, to investigate how the gene therapy is distributed to further improve therapy delivery and device design in future trials.
As a Clinical Research Fellow in Neurosurgery, Susruta is working on identifying strategies for optimising the effective delivery of cell and gene-therapies to the brain, under the supervision of Professor Liam Gray.
About me
I am a neurosurgical trainee currently taking time out of my programme to develop my academic training with the BRAIN Unit.
I was keen to return to BRAIN’s excellent environment for translational neurosurgical research, having completed my undergraduate and early-postgraduate medical training at Cardiff University.
The research
Cell and gene-based therapies, collectively known as advanced therapy medicinal products (ATMPs), are expected to revolutionise the treatment of neurological disorders in the upcoming future.
Following decades of pre-clinical investigation, we are at an exciting transition towards ATMPs entering clinical transplantation trials for debilitating neurological disorders such as Huntington’s Disease (HD), Parkinson’s Disease (PD) and temporal lobe epilepsy (TLE). In such diseases, ATMPs must be delivered surgically to specific targets within the brain.
Initially considered to be a trivial problem, achieving effective direct delivery is now recognised as a significant obstacle to treatment success. This is due to the hostile micro-environment arising from a complex combination of surgical delivery, the pre-existing disease, and the patient’s immune response to ATMPs.
Our research is focused on understanding how these inter-related factors can be modified to ensure that ATMP efficacy is maximised. This will require investigation using a series of different models.
Firstly, we will use a transgenic HD model to identify pro-inflammatory cell signalling pathways that are activated after surgical delivery procedures. We can then study the effects of modifying signalling pathways anticipated to have negative effects on ATMP success.
Secondly, we will use an established three-dimensional cell culture model (‘Hi Spot® model’), generated from human brain tissue collected from patients undergoing specific neurosurgical procedures. Comparing ATMP delivery in ‘control’ cortical Hi Spots with sclerotic hippocampal Hi Spots can provide valuable insight into the innate immune response to ATMPs in the inflamed micro-environment.
Research implications
We anticipate that this work will answer crucial questions regarding the ‘science of ATMP delivery’ and pave the way towards more successful treatment of currently incurable neurological disorders in the upcoming era of regenerative neuroscience.
May 2023 was a busy month for the BRAIN Unit, from science talks science to hosting the highly anticipated BRAIN games, with primary school attendees from across Cardiff. Read on to find out more.
Science with a pint: hearts and minds research
On May 5th, BRAIN researchers Professor Anne Rosser and Dr Emma Lane hosted a ‘Hearts and Minds’ event in Radyr Golf Club. Attendees had the opportunity to hear about the latest research and clinical developments in neurological diseases and cardiology and take part in demonstrations. The night saw some amazing talks, including one from Dr John Huish who talked about the history of cardiology. Interventional radiologist, Chris Williams brought a range of stents for attendees to try and deploy, as well as rat brain sections which were stained to reveal dopaminergic transplants – displayed under a microscope!
Exploring the effects of samba on neuroplasticity in Parkinson’s disease
May 13th saw Parkinson’s researchers from Bangor, Cardiff and Swansea come together to host simultaneous events, along with the Wales Research Interest group. One of the events was funded by the Dementia Research Institute and the BRAIN involve group, both based in the Hadyn Ellis Building (HEB) at Cardiff University. Around 100 people with Parkinson’s and their family members came to HEB to hear about the latest research in Parkinson’s disease and see the launch of an all-new samba group for people with Parkinson’s: ‘SParky Samba’.
‘SParky Samba’ aims to develop strong community bonds between those with lived experience of Parkinson’s as well as explore the benefits of Samba percussion in promoting neuroplasticity. It is facilitated by a local Cardiff-based Afro Brazilian percussion band named Barracwda. You can find out more about SParky Samba by following them on Twitter.
Promoting equality and diversity in research
Dr Emma Lane was invited to speak at two events hosted by the Equality Diversion Inclusion in Research (EDIRA) project group on 12th and 19th May. EDIRA aims to create an inclusive research framework, developing guidance using the perspectives of underserved communities and supporting the work of professionals from various Communities of Practice.
Another year, another BRAIN Games for primary pupils
On May 19th, 4 Cardiff primary schools visited two of Cardiff University’s research facilities: Spark and CUBRIC to learn more about brain research and take part in a variety of fun brain-related activities.

Researchers at Cardiff University have been awarded funding that will enable them to better map the brain to treat diseases such as epilepsy, dementia, and multiple sclerosis.
A £1 million grant from the Medical Research Council was secured by Cardiff University, along with University College London, Leeds and the University of Cape Western Reserve. The Cardiff University team includes Professor Derek Jones, Professor Liam Gray, Khalid Hamandi and Dr Marco Palombo.
The grant will enable researchers to ‘make the invisible visible’ by obtaining high-quality images of the human brain and learning the mapping between Magnetic Resonance Imaging (MRI) and histology, the microscopic study of human tissue.
Making the invisible visible
Professor Liam Gray explained, “One of the key challenges in diagnosing brain disease such as epilepsy, dementia or multiple sclerosis is the difficulty in detecting small and subtle cortical abnormalities that are not easily identified. Conventional MRI scanners can detect abnormal signals, but it’s impossible to tell what’s driving them; this could be differences in cell size, shape or density. Currently, such information can only be obtained by cutting the tissue and examining it under a microscope.”
Examining the cortex using state-of-the-art equipment
The funding will enable researchers to take advantage of advances in MRI physics, which hold the promise of detecting and characterising tissue abnormalities that are currently “invisible”. Such technologies have been applied to the examination of white matter, which is associated with psychiatric diseases such as schizophrenia, but the cortex remains unexplored to an extent.
To illuminate infected tissue, BRAIN researchers will scan patients in state-of-the-art equipment, remove pathological tissue through surgery, transport it to an experimental MRI scanner for extended scanning, and then light microscopy and electron microscopy will be used. These techniques allow us to see the brain over a variety of scales of magnification.
This will allow us to establish an MRI signalling ‘fingerprint’ of specific disease processes in the cortex that are currently invisible to conventional MRI, creating a significant change in our ability to localise pathologies in the brain and monitor them non-invasively over time.
Funding research opportunities
The grant will also fund an 18-month Clinical Research Fellow in an Experimental Functional Neurosurgery position. The Clinical Research Fellow will be responsible for preparing and recruiting study participants as well as dealing with and processing surgical tissue during the study.
Professor Gray will carry out surgery to extract tissue samples from patients, who will be anonymously linked to the work so data can remain confidential. It is then processed in the Human Tissue Laboratories of the BRAIN Unit at the University Hospital of Wales (YAC). Samples will then be sent to colleagues on the MRC grant who will scan the tissue and process it for Immunohistochemistry (IHC) and electron microscopy which will show disease evidence that will be mapped to the Magnetic Resonance Imaging (MRI).
Professor Liam Gray said, “If successful, this technology could help us localise the cortical pathology that causes epilepsy in the brain and allow surgery to be more accurately targeted to cure epilepsy. It could also significantly expand the population of patients suitable for surgery.”
Dr Benjamin Dummer is a Research Assistant based in a lab at the University Hospital of Wales (UHW), under the supervision of Professor Liam Gray.
The research
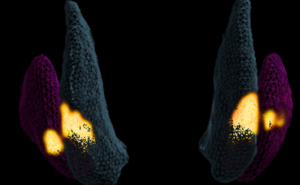
Our current research focuses on glioblastoma, which is a deadly brain cancer. We are characterising a 3D cell culture model using brain tumour tissue direct from surgery. This will allow us to personalise medicines to individual patients and gain a better understanding of glioblastoma biology.
We are also collaborating with other research groups within Cardiff University and outside institutions to explore how our 3D model can be used to better understand other neurological diseases.
Despite decades of research and millions of pounds spent, patient outcomes for people diagnosed with glioblastomas is still very poor. There is a clear need for developing novel treatments to combat the disease. Within these tumours there is a subpopulation of cells called stem cells which are implicated in treatment resistant and disease progression. Understanding how these cells interact with each other and their microenvironment is a fascinating area of research which will hopefully lead to a better understanding of this deadly disease.

What next?
Our next step is to complete the work on our 3D model so we can move forward to developing a personalised medicine paradigm with the aim of helping patients who suffer with this horrible disease.
BRAIN researchers have co-edited a book which examines the progress of cell therapies in the treatment of neurodegenerative diseases, published last November.
Cell therapies are a promising development for the treatment of neurodegenerative diseases (NDDs) such as Huntington’s and Parkinson’s, which occur when nerve cells in the brain or the nervous system stop working or die.
The symptoms of NDDs are varied and can range from memory loss and mood disorder to mobility issues. Existing medicines for NDDs aim to minimise some of these symptoms but are unable to treat the root causes of the disease itself.
New therapies such as Advanced Therapeutic Medicinal Products (ATMPs) are a new and personalised alternative to treating NDDs. Unlike existing medicines, ATMPs aim to treat the direct cause of disease whereby cells, protein, or DNA is extracted from a patient before they are altered and then re injected.
The BRAIN Unit, based at Cardiff University is examining the effects of ATMPs in a series of clinical trials. Clinical trials enable researchers to test the effectiveness of a new treatment and ensure it is safe enough to use on a wider scale.
The new book, ‘Current Challenges in Cell Therapy for Neurodegenerative Diseases’ is co-edited by three of BRAIN’s researchers: Emma Lane, Mariah Lelos and Cheney Drew and was commissioned as part of the International Review of Neurodegenerative Diseases. The book examines the progress of such ATMPs, as well as some of the challenges of translating these therapies into a clinical setting.
As well as editing the volume, Lane, Lelos and Drew also contributed chapters to the book, aligned with their current areas of research. This includes the development of stem cell therapies for Parkinson’s and Huntington’s disease and how those are investigated with the use of animal models, how we can evaluate ATMPs in clinical trials and the importance of including the patient voice in the development and testing of new treatments.

Cheney Drew said, “We are delighted to bring together leading international experts in the development and clinical translation of cell and gene therapies in neurodegenerative disease. The contributions to this volume cover the breadth of novel cell and gene therapy development and evaluation across a number of neurodegenerative disorders.”
‘Current Challenges in Cell Therapy for Neurodegenerative Diseases’ is available to purchase in hard cover or ebook format.
Lauren Griffiths is a Research Technician at Swansea University. Her recent research has centred around cholesterol, its function in the brain, and understanding its role in neurodegenerative diseases.
Cholesterol is an essential molecule in the body, and especially in the brain, where it is the most common lipid and is essential for cell membranes, including the myelin sheath (the fatty substance that allows nerve signals to move quickly).
The synthesis and metabolism of cholesterol are regulated by enzymatic reactions, but what happens when this process goes wrong and how does it impact brain function?
The research
That was the question I wanted to answer when beginning my PhD almost four years ago, where, as part of the team that developed a novel imaging technique that, paired with mass spectrometry, allows us to accurately map and measure cholesterol across intact brain tissue sections.
This method of mapping and measuring cholesterol in the brain was the first of its kind and has come at a really important time where interest has turned to how cholesterol, and its derivatives, play important roles in neurodegenerative diseases like Alzheimer’s, Parkinson’s, and Huntington’s.
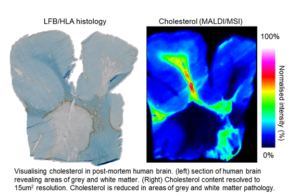
We have recently applied our method of imaging cholesterol to human multiple sclerosis (MS) tissue and collaborated with the Brain Repair Group in Cardiff University (Prof Anne Rosser and Dr Mariah Lelos) to analyse cholesterol in the brain of Huntington’s disease (HD).
What next?
The next steps in our research journey with BRAIN are to analyse the cholesterol precursors and derivatives, the oxysterols, using another novel mass spectrometry technique. Oxysterols are important signals to protect neurons from dying and reduce brain inflammation.
One important oxysterol that we are now focussing on is 24S-hydroxycholesterol, which is linked to neuronal loss and when its synthesis is boosted can prevent neurodegeneration in animal models.

Around 145,000 people live with Parkinson’s in the UK, and it’s the fastest-growing neurological condition in the world. For World Parkinson’s Day, Dr Emma Lane from the BRAIN Unit discusses the disease and some things you may not know.
What is Parkinson’s disease?
Parkinson’s disease is a neurological condition that causes progressive damage to the brain over many years. People with Parkinson’s don’t have enough of the chemical dopamine because some of the nerve cells that make it have died.
There are lots of different treatments and therapies available to help manage the condition.
It affects around one in 500 people but this increases with age, rising to one in 100 people over 60 years old and 3 in 100 people over 80. Symptoms can include tremor, slow movement and stiff and inflexible muscles.
People with the condition may also experience mental health problems such as depression and anxiety.
Facts about Parkinson’s disease
While Parkinson’s diagnoses continue to increase around the world, it’s not always the most understood condition.
1. Parkinson’s has a scent
There are some people who can actually ‘smell Parkinson’s’ and this has led to some brilliant research into how the skin may be affected by Parkinson’s and whether this can be used to detect the disease. In contrast, another symptom of Parkinson’s can be the loss of smell of certain foods like bananas, dill pickles, and liquorice.
2. Parkinson’s is more than ‘just’ a motor condition
Nonmotor symptoms are getting more attention from doctors and researchers. These symptoms include but are not limited to, cognitive impairment or dementia (usually in later stages), anxiety, depression, fatigue, and sleep problems.
For some patients, nonmotor symptoms are more disabling than motor symptoms, which are the focus of treatment.
Be sure to talk to your doctor about other issues so you can get all of your symptoms addressed.
3. Parkinson’s is not a fatal disease
Although a diagnosis of Parkinson’s is devastating, it is not, as some may still believe, a death sentence.
Parkinson’s disease is not a direct killer, like stroke or heart attack. Much depends on the quality of your care, both from your doctor and yourself. There are some very good drugs that help manage many of the symptoms.
The gait and balance changes may make you more vulnerable to falls. These are reasons why exercise and physical therapy are so important.
4. No two people have exactly the same symptoms
The progression of symptoms is often a bit different from one person to another due to the diversity of the disease and changes as the disease progresses.
Many people think of Parkinson’s as the ‘one where you shake’. In fact, only about a third of people experience tremors as part of their disease.
People with Parkinson’s may experience slowness of movements, limb rigidity, changes in the way they walk, and problems with balance.
A change in handwriting, specifically handwriting that’s become smaller or more crowded, or a less expressive face, are also symptoms.
5. The cause is unknown and there is currently no cure
What causes Parkinson’s remains largely unknown.
Genetics cause about 10 to 15 percent of all Parkinson’s. The other 85 to 90 percent of cases are classified as ‘sporadic’ or ‘occasional’.
Although there is currently no cure, which organisations like Parkinson’s UK are working to change, treatment options vary and include medications and surgery.
6. Running or walking?
People with Parkinson’s often find other forms of activity easier than walking.
Running or riding a bike can be easier than walking.
Getting through doorways can be a particular challenge and people with Parkinson’s have strategies to deal with circumstances that make them ‘freeze’ at lines on the carpet or doorways.
7. What you eat makes a difference
The drugs that treat Parkinson’s disease help replace the chemical in the brain, dopamine, that is lost as the brain cells die. This can work very effectively but it can be improved with changes in diet.
High levels of protein in the diet can stop the drugs from getting to the brain to do their job, so managing when and what you eat around your medication can make a huge difference to their effects.
8. Treating Parkinson’s
For people with Parkinson’s, exercise is more than healthy, it’s a vital component of maintaining balance, mobility, and activities of daily living.
Exercise and physical activity can improve many of its symptoms. A minimum of two and a half hours a week can slow the decline in quality of life.
Tai chi, yoga, Pilates, dance, weight training, and non-contact boxing can all have positive effects.
Your Parkinson’s specialist will be able to support the management of your symptoms with medication and guidance for other forms of support
Seeking medical advice
If you’re concerned that you or someone you know may have symptoms of Parkinson’s disease then it’s advised to see a GP.
They’ll ask you about the problems you’re experiencing and may refer you to a specialist for further tests.
Work at the BRAIN Unit
Dr Lane concludes: “10 years ago, commercial research into neurodegenerative diseases was struggling. There has been a huge shift recently with several exciting and diverse approaches to treating Parkinson’s reaching clinical trials.
“At the Brain Unit, we are passionate about ensuring our patient community voices are heard as part of these exciting developments and they are on this journey with us in the search for effective treatments.”
Learn more about work underway with BRAIN Involve, the BRAIN Unit’s public and patient involvement group made up of people who are, or have been, affected by neurological diseases.



