Meet the researcher: Dr Malik Zaben
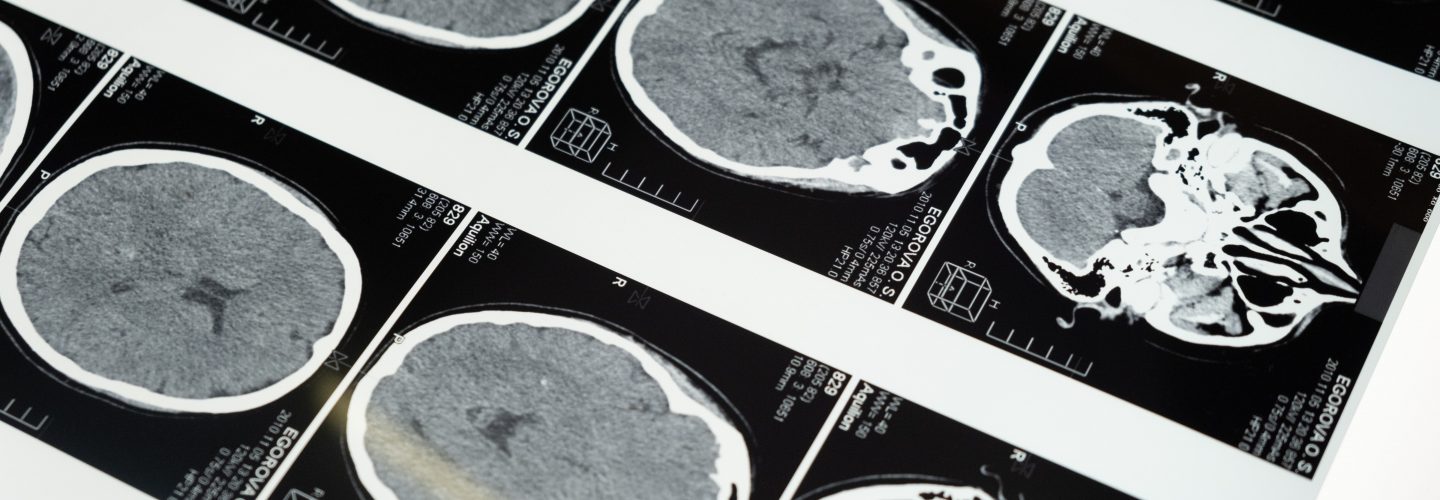
Dr Zaben is a lecturer in neurosurgery with a special interest in understanding neurogenesis and neuroplasticity after traumatic brain injury (TBI). His research explores potential therapeutic approaches targeting neuroinflammatory pathways to limit brain damage after injury, and enhance repair.

This year has been another successful one for our Traumatic Brain Injury research team at Cardiff University, despite the challenges that the COVID-19 pandemic has caused.
We have been able to address some new facets of our research area covering the broad spectrum of basic science and clinical research.
The research
The COVID-19 pandemic meant that we had to leave the laboratory in mid-March of 2020 and were not able to return until mid-July.
Despite this major disruption, we are now able to continue our research in-house. Building on our previous findings, we have generated novel and relevant data on the inflammatory pathways triggered by seizures and Traumatic Brain Injury (TBI), which are heavily implicated in long-term neurocognitive deficits in patients from both categories.
Our key target of interest is HMGB1, a protein that is released by immune cells significantly after epilepsy and TBI and increasingly recognised as the ‘master switch of neuroinflammation in the acute phase after injury.
Elevated levels of HMGB1 in the blood of patients with TBI are associated with worse outcome in patients with epilepsy as well as TBI. Blocking this protein in a time-specific manner may hold the answer to ameliorating the neuro-toxic milieu created after injury and improving brain repair.
Whilst we previously observed a significant release of HMGB1 after injury, we have now discovered that HMGB1 has a detrimental effect on neural stem cells’ ability to generate new neurons or repair nerve cell fibres after injury.
This year we have also identified the receptors and pathways involved in the above-mentioned effect and, more importantly, managed to reverse HMGB1 effects using some novel drug strategies.
These findings pave the way for identifying potential drugs that can be used to enhance nerve cell repair after injury.
We have now published some of our key findings in two peer-reviewed papers in the Journal of Brain Science and Journal of Scientific Reports.
We have submitted our work on pathways involving HMGB1 and other inflammatory cytokines involved in epilepsy for publication at the Journal of Neuroinflammation (under revision).
What next?
Moving forward, we will be validating our findings in human brain tissue. With the consent of patients undergoing neurosurgery, we will obtain small samples of normal brain tissue that would otherwise have been discarded as a routine part of the surgery.
We can then grow these cells in a specialised 3D in vitro culture system that closely mimics their natural parent environment in vivo. With judiciously calculated weight drop injury models; we are studying the effects of blocking HMGB1 on improving brain repair after injury.
With evidence from both rodent and human tissue, we hope to elucidate the potential detrimental role of HMGB1 in TBI and provide promising therapeutic targets for improving outcomes in TBI patients.
We continue to make exciting progress and we are incredibly grateful for our funders’ continued support.